Breakthroughs in Alzheimer’s Disease Research: A Ray of Hope
While it may feel hard to ignore the harsh realities that accompany dementia, there are some pockets of good news on the horizon. Seniorly shares 5 reasons we're feeling hopeful about Alzheimer's research.
While dementia remains the seventh leading cause of death worldwide, promising research shows how dedicated we are to understanding brain health and dementia. These new developments offer a bright, hopeful glimpse at how we'll handle this challenge in the future. With that in mind, we're excited to share some news from recent research efforts that is giving us a reason to feel optimistic.
Dementia and Alzheimer's disease: a primer
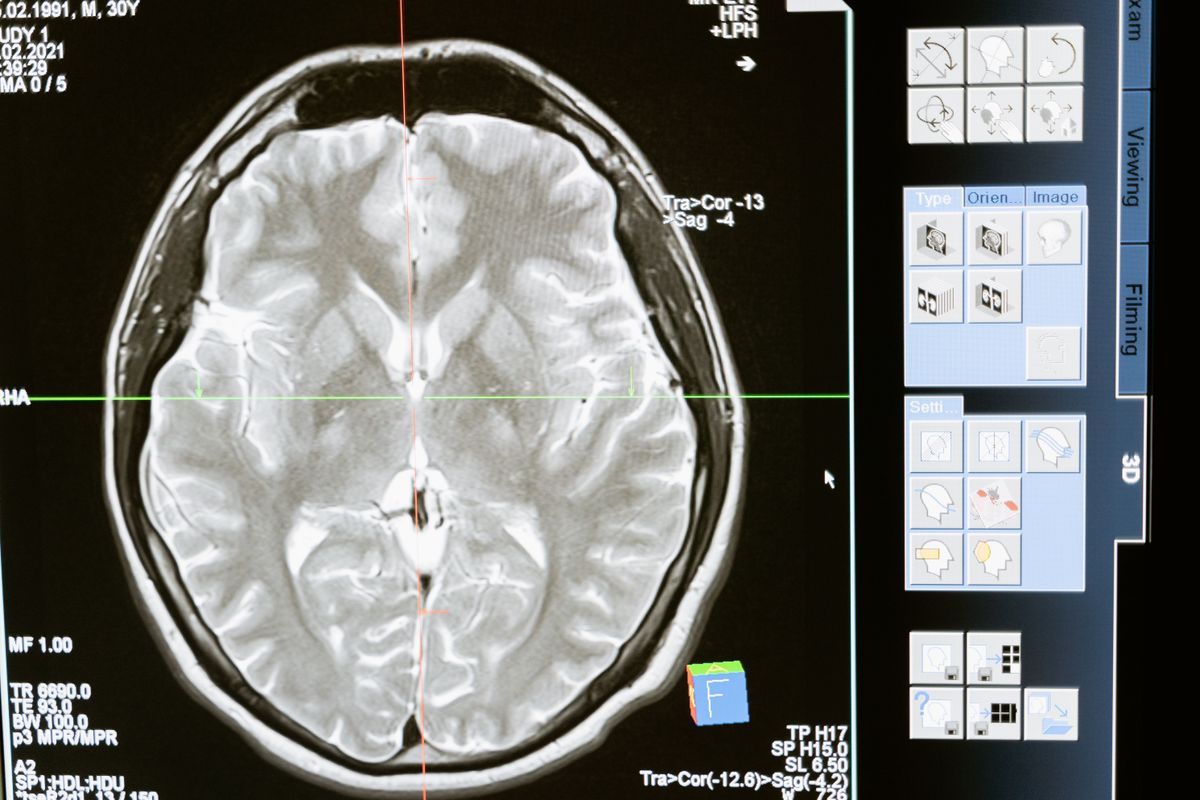
Think of your brain as a bustling city, filled with complex paths, roads and superhighways - where thoughts, memories, and commands are like cars moving throughout. Now, dementia is a bit like a persistent traffic jam in the city. It causes problems in at least two different brain activities, like memory, language, reasoning, or visual perception, making it harder for your thoughts to get to their destinations. It's the umbrella term we use for conditions that cause these symptoms.
Alzheimer's Disease is the most common cause of dementia, much like a notorious bottleneck causing a lot of our traffic jams. It's where an abnormal protein surrounds brain cells and another protein damages their internal structure. Essentially, it's like part of our city is being damaged and falling apart, and as a result, the beautiful complexity of our brain isn’t running as smoothly as it once was.
Fighting a complex disease
While we have made significant strides in understanding dementia, a definitive cure continues to elude us. One key reason is the sheer complexity of the brain. With billions of neurons and an unfathomable web of connections, the brain presents a profound mystery that we've only just begun to unravel.
Dementia isn't just a single disease but a collection of symptoms that occur when brain cells stop working properly; it's a common effect of various diseases, most notably Alzheimer’s. Because the causes of these diseases are so diverse, finding a 'one-size-fits-all' cure is extremely challenging. The brain's natural defense mechanisms create a unique challenge, as these barriers often prevent potential drugs from reaching their targets. The slow progression of the disease also makes it harder to measure whether potential treatments are effective. Another reason is that we don’t quite know what is causing the traffic jam, in the first place, which makes finding a cure that much harder.
The Alzheimer's research community also faces ethical issues, particularly when studies involve people with severe or even mild cognitive impairment. Despite all these hurdles, our drive to advance dementia research remains unshaken, instigated by the urgent need to understand this complex condition better.
Who funds research on Alzheimer's and related dementias?
It should come as no surprise that funding for dementia research comes from various sources; after all, a disease this complex requires a collaborative effort. Government agencies like the National Institutes of Aging (NIA) at the National Institutes of Health (NIH) in the U.S and National Institute for Health Research (NIHR) in the UK are significant contributors to clinical research, with substantial budgets for dementia-related research.
Foundations such as the Alzheimer's Association, Alzheimer's Research UK and Alzheimer's Society also provide considerable resources to foster research, while pharmaceutical companies also invest heavily in the exploration and development of new treatments.
Universities and private research institutions contribute to drug development as well, typically through grants or partnerships. Finally, generous donations from individuals and philanthropic organizations play a crucial role, particularly in funding early-stage, innovative research. These sources combine to form a solid financial backbone, crucial in driving the relentless pursuit to demystify and defeat dementia.
5 reasons to be excited about Alzheimer's research
1) WHO's blueprint for dementia research
Background: The World Health Organization (WHO) is deeply involved in Alzheimer's disease and dementia planning and research due to the global prevalence and serious impact of the disease. As an international public health agency, the WHO is committed to promoting health, keeping the world safe, and serving vulnerable populations, tasks that all encompass addressing dementia. Given the fact that dementia does not recognize borders and impacts people everywhere, it falls within the WHO's mandate to coordinate worldwide research studies and efforts against the disease. The WHO is uniquely equipped to bring together researchers, governments, and other stakeholders from all over the globe, fostering collaboration and ensuring best practices are shared in order to accelerate progress in dementia research.
Why we're excited: The World Health Organization developed a blueprint to integrate and strengthen global Alzheimer's disease and dementia research efforts. This document, a first of its kind for noncommunicable diseases, offers guidance for policy makers, funding bodies, and researchers, aiming to make dementia research more efficient, fair, and effective. The blueprint not only applies lessons from WHO's research on infectious diseases but also considers the whole spectrum of dementia research, from diagnostics to new scientific and technological developments. It provides insights into various drivers of research, such as sustainable funding, inclusivity, and the involvement of those with lived experiences of dementia. With such a wide-reaching and influential body helping to coordinate and lead the fight, we're feeling optimistic about what lies ahead.
2) Amyloid immunotherapy
Background: The amyloid-beta is a protein that naturally exists in the brain. In a healthy brain, these proteins are broken down and removed. But in a brain affected by Alzheimer's disease, in accordance with a popular hypothesis, these proteins appear to clump together to form 'plaques'. These plaques are believed to block communication among neurons, which are crucial for memory, thoughts, and feelings. Essentially, some experts believe that the build-up of amyloid-beta proteins disrupts the normal functioning of the brain, contributing to the symptoms commonly associated with Alzheimer's disease such as memory loss and cognitive decline. However, the exact role of these plaques in the disease process is still under intense scientific study.
Why we're excited: Recent clinical trial therapies targeting the amyloid protein have been undertaken by a few organizations. If we can figure out how to manage the protein, we may be able to prevent Alzheimer’s disease progression. It's not light reading, but you can check out briefs from research below:
3) The COVID connection
Background: Those who have contracted COVID-19, especially severe cases, have sometimes reported lingering 'brain fog', cognitive difficulties, and other neurological symptoms post-recovery. Scientists now have the opportunity to do further research to examine the connection between COVID and Alzheimer's disease and dementia.
Why we're excited: Scientific studies are currently investigating whether individuals who've had COVID-19 may have an increased risk of developing Alzheimer's or other forms of dementia in the long term due to the virus's impact on the brain. There may be a link between COVID infection and the presence of Alzheimer’s-like biochemical changes in the brain. There is also emerging work that examines a link between viral diseases and various neurodegenerative diseases later in life. As with all research related to dementia, it's important to note that much more research is needed to establish definitive conclusions.
4) Early detection of Alzheimer's
Background: Early detection of Alzheimer's presents a challenge largely due to the insidious nature of the disease. In its early stages, Alzheimer's can present as mild forgetfulness or confusion - symptoms that can easily be dismissed as part of the normal aging process, or even stress. Initial symptoms can vary greatly between individuals, and there's currently no single test to definitively diagnose Alzheimer's. To top it off, the changes in the brain associated with Alzheimer's can begin years, even decades, before symptoms appear. This means the disease can advance silently, accumulating damage before noticeable cognitive decline surfaces. Together, these factors contribute to the difficulty of early detection, underscoring the need for more research on early biomarkers and screening strategies for Alzheimer's.
Why we're excited: In the last few months, research on signals in the blood are emerging as promising methods to detect the disease in its early stages. As we mentioned earlier, amyloid plaques in the brain are a key hallmark of Alzheimer's disease, but until recently, detecting these plaques generally required expensive PET scans or invasive spinal taps. The development of blood tests that measure certain forms of amyloid protein has the potential to revolutionize this process. These tests could theoretically detect changes in amyloid levels years before noticeable symptoms start, allowing for early intervention and potentially slowing disease progression. Not only do these tests raise the possibility of more accessible and timely diagnosis, but early research suggests they could also predict who will develop Alzheimer's with a high degree of accuracy. It’s an exciting development, although more research is needed before such tests are ready for widespread clinical use.
5) Managing agitation in Alzheimer's patients
Background: Agitation is a common behavioral symptom in people with dementia, and it can significantly impact their quality of life - not to mention that of their loved ones. It usually manifests as restlessness, emotional distress, aggressive behaviors, or resistance to care. Agitation in dementia is thought to be caused by a combination of factors, including brain changes due to dementia that affect mood and behavior, unmet needs (like pain or hunger), or environmental factors, such as excessive noise or lack of routine. For those living with dementia, bouts of agitation can be extremely distressing and disorienting, causing heightened anxiety or fear. It also poses challenges for caregivers, family members and healthcare providers, often requiring specialized training and interventions to effectively manage.
Why we're excited: The U.S. Food and Drug Administration (FDA) recently gave its approval for the use of Rexulti (generic name: brexpiprazole) as a treatment to manage agitation in patients with Alzheimer's disease. This approval is a significant milestone in dementia care, as agitation is a common and distressing symptom that can dramatically impact the quality of life for patients and caregivers. Rexulti's approval is based on positive results from clinical trials, which demonstrated the drug's effectiveness in reducing episodes of agitation. Its mechanism involves modifying the activity of certain neurotransmitters in the brain, which are thought to play a role in agitation.

While we may not yet have all the answers when it comes to dementia, recent research presents a beacon of hope. From ground-breaking studies on early detection methods to promising advancements in treatment options, scientists around the globe are unrelenting in their pursuit of a cure. Each step forward in dementia research not only broadens our understanding of this complex condition but also brings us closer to a future where dementia becomes a manageable, perhaps even preventable, condition. In this era of dynamic scientific exploration, it is clear that the fight against dementia remains a global priority.
Works consulted:
Marlena del Hierro earned her Master of Arts degree in Gerontology from San Francisco State University and her Bachelor of Arts degree in Human Development from California State University. She also serves in an advisory capacity for Jukebox Health. Marlena is a vocal advocate for evolving the aging paradigm, and is a frequent contributor to public discussions about aging. She has served as a resource for media outlets like WGBH, FOX News, CNBC and the Today Show.
To learn more about Seniorly's editorial guidelines, click here.
Sign up for our Healthy Aging Handbook
Seniorly’s Senior Living experts created a comprehensive handbook to help people age happily while ensuring they love where they live. Enter your email address below to receive your copy and learn more about Healthy Aging and Senior Living.*
*By submitting your email address above, you consent to receive occasional email communications from Seniorly, including educational content and tips, newsletters, and other relevant updates and offerings. You can unsubscribe at any time and we will never sell or distribute your email address to a third party. You can view our Privacy Policy here.
